
Food sensitivities: don’t take them lightly
For a few years, we’ve known that my daughter Eva got periodic stomach aches when she ate gluten or sugar. It wasn’t every time, but regularly enough that even a then 14 year old saw the connection.
As a nutritionist, I’ve learned that the “gold standard” for identifying food sensitivities is an elimination diet. If we feel better without a food: take it out, regardless of what a test result is telling you. During an elimination diet, a person removes a suspect food completely from the diet for two to three weeks in order to test the body’s reaction to the food when reintroduced. When an offensive food is out of the body, the immune system has a chance to calm down. Then, if a food really is activating the immune system, when the food is added back in, there will be some kind of immune reaction.
Given that Eva’s stomach aches are very typical in my clientele, I felt confident that we’d eliminate a couple of obvious foods first (gluten and dairy) and get to the bottom of her gut issues. She felt significantly better without gluten and sugar and we discussed that she’d eliminate them.
The tricky thing about identifying food sensitivities (different from a food allergy) is that a reintroduction of a food after elimination does not necessarily cause an immediate reaction such as a classic food allergy does. Food sensitivities do not activate an IgE immune response which results in immediate swelling, hives, etc. Instead, a sensitive food might cause trigger an IgM, IgA or IgG immune response, which can occur up to 72 hours after the offending food is ingested. To further complicate the identification of a food sensitivity, we must look for reactions that don’t always include digestive symptoms. Food sensitivities can cause a reaction in any system of the body. Common reactions include headaches, brain fog, muscle aches, skin reactions, anxiety, congestion, and chronic pain in addition to digestive responses like gas, bloating, constipation, and diarrhea.
Identifying food sensitivities is a major part of the work I do with clients. Typically, my clients DO find that eliminating certain foods relieves chronic symptoms. I’ve worked with so many clients who have had long term acne, chronic congestion, anxiety, brain fog, hay fever, migraines, swelling, weight loss resistance (and more) disappear or significantly improve after eliminating their sensitive foods. By the way, the most common food sensitivities are to gluten, dairy, soy, corn, and eggs, but a person can be reactive to any food.
Although Eva had clear reactions to both gluten and sugar, she didn’t totally understand the importance of being consistent with her avoidance of them. When Eva felt poorly, she’d be consistent, but as her symptoms improved, her resolve would fade. She’d eat great at home, but if she was with her friends, she’d nibble on whatever was around if she was hungry enough. Then she’d end up feeling poorly, swear off gluten and sugar and the cycle would continue. Totally normal, right?
What happens when you continue to eat a food that causes an immune reaction?
Fast forward three years of being inconsistently “gluten free.” This spring, Eva seemed to be feeling ill regularly. We also noticed that there were more foods that made her feel instantly “sick.” The kid eats better than any teen I know. But still, oatmeal gave her headaches. Yogurt made her gut hurt. We spent a few days on the road over spring break and she barely wanted to eat because everything made her feel sick. We were both scared at this disintegration of her health.
Testing
With college looming ahead of us (she just finished her junior year), and with her rapidly increasing food reactivity, we knew we needed help. Eva needed to hear from someone other than her mom that she needed to be consistent with gluten/sugar elimination, but we also needed to get to the bottom of what these new reactions were about. We consulted with a fabulous functional doctor. We did some food sensitivity testing (which are different than a typical allergist would offer) and were overwhelmed to see the list of foods to which she was reacting. Some were completely random: Carob? Catfish? Others weren’t so surprising to me: gluten, dairy, soy.
And this is where I get to the point of this story.
Leaky Gut
Whether we know it or not, our health is heavily dependent upon the health of our intestinal tract. Part of this tract is the small intestine, which is primarily responsible for the absorption of nutrients we ingest.
The nutrients in our food are not ready to be absorbed into our bloodstream until they are broken down into particles that our immune system won’t regard as foreign. For example, even though we might eat ground beef, we couldn’t inject ground beef into our bloodstream or our immune system would go haywire, right? It needs to be digested first.
So if all is working well, carbs are broken down into glucose, proteins into amino acids and fats into free fatty acids. At only this point of digestion should these particles seep through the teeny cracks between the cells of our small intestine lining into our bloodstream, where they are ushered into our cells to do their work. Make sense?
If we’re eating food that we are not breaking down properly, these food macromolecules can irritate the gut, which ultimately can result in inflammation of the gut lining. Gluten is notorious for being difficult to break down in the gut. Inflammation (also caused by NSAIDS, alcohol, stress, steroid medications, chemotherapy), can loosen the spaces between the cells of the intestinal walls. Because of this loosening of these tight cellular junctures, macromolecules can seep through the intestinal wall into our bloodstream.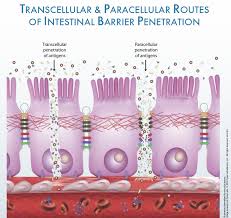
This is where the immune system kicks in. If a macromolecule of food gets into the bloodstream, the immune system doesn’t recognize it as safe. It attacks (i.e. inflames). Our immune system has a memory (which is exactly why vaccinations work): the next time a macromolecule from that particular food seeps through the intestinal wall, the immune system will react again, attacking it as an antigen.
This is the beginning of a food sensitivity. If unrecognized food sensitivities are creating leaky gut (also known as intestinal permeability), and the same foods are consumed over and over, a self- perpetuating, inflammatory cycle will be triggered, and the intestinal lining cannot heal. Not only that, but this inflammation is systemic. Inflammation is the bedrock for most diseases: Alzheimer’s, cancer, arthritis, acne, even depression can be rooted in inflammation. We do not want to be on fire.
Eliminate and don’t look back
I’m convinced that had we had Eva tested two years ago, the list of irritating foods would have been much smaller. Yet with ongoing (albeit infrequent) exposure to gluten, her gut never had a chance to heal. Instead, the ongoing inflammation resulted in increased leakiness, and thus the list of offending foods grew.
Why is it important to be consistent? Well, the more conservative estimates are that inflammation triggered by offensive foods can last as long as 6 months. So, a little bite of dairy here and there if you’re sensitive can result in a long, slow inner fire. If you know you react to a food, please don’t be casual about “cheating” now and again.
What now?
Happily, the gut can heal, but not without eliminating the foods that are triggering the immune system. Removing the offensive food is the first step to healing. The sooner we act, the more damage we can prevent, and the easier it will be to heal. Although some food sensitivities are permanent, it is possible to improve gut health so that a person does not end up with a laundry list of foods to avoid. I’m confident that Eva’s diet will become much less restrictive. We will retest in a few months. Already, after one month of total vigilance and going on an ambitious gut healing protocol, she’s feeling a lot better day to day.
Please let me know if you need help identifying food sensitivities or want support in healing your gut. Not only is it important to remove the foods, but restore the gut through a gut-healing protocol. I’ll tell you more about this protocol in a future newsletter.



